Metabolic factors and the risk of Dupuytren’s disease: data from 30,000 individuals followed for over 20 years
The findings from this longitudinal population-based study with a median follow up of 23 years corroborate that DM and excessive alcohol consumption constitute major risk factors for the development of DD. Furthermore, we found an inverse association between obesity among men and DD. We also present data proposing an inverse association between ApoB/ApoA1 ratio and DD, findings that has not been previously reported. In addition to information regarding risk factors for DD, the study sheds light on the complex associations between DD, DM, and high BMI.
Diabetes Mellitus
DM has long been considered a risk factor for DD, although the exact mechanisms by which hyperglycaemia affects the palmar fascia are still not fully understood1,10. One of the proposed biochemical processes underlying diabetic complications is the formation of advanced glycated end products (AGEs)18. AGEs have been associated with other fibroproliferative disorders, such as diabetic cardiomyopathy19 and idiopathic pulmonary fibrosis20, but also to complications of diabetes in the hand, e.g. carpal tunnel syndrome21. Indeed, data from biopsies from the palmar fascia in patients with DD showed higher levels of AGEs compared to a control group22, possibly increasing levels of collagen deposition and increased collagen stiffness10,22. Furthermore, previous studies have shown that DM increases the formation of myofibroblasts23, one of the proposed main cell types responsible for contraction the finger in DD24. Thus, future studies should examine the palmar fascia in patients with DM to clarify the effects of hyperglycaemia and AGEs on the development of DD. In our study, participants with prevalent DM at baseline had marked increased risk for development of DD during follow-up; even when adjusting for other known risk factors, e.g. alcohol consumption and BMI. Our results are in line with a previous meta-analysis on the effect of DM on the development of DD10. Our study adds important information due to its longitudinal setting and long follow-up, why it contributes to the establishment of DM as a major risk factor for the development of DD. Finally, our findings support the theory of DD as being a part of the more complex syndrome—“the diabetic hand”, together with diagnoses, such as carpal tunnel syndrome, trigger finger, and ulnar neuropathy25,26,27.
Alcohol consumption and manual work
In our study, excessive alcohol consumers of both sexes had a marked higher risk of developing DD during follow-up, and these results are in line with several previous studies linking alcohol overconsumption to the development of DD5,6. Alcohol guidelines and thresholds for risk consumption differ notably from country to country28, but our study shows that already a somewhat moderate alcohol consumption (1–2 standard drinks per day), well below the definition of low-risk consumption in some countries29, is associated with an increased risk of DD. By adding long term follow-up data, our study strengthens the previously reported associations, establishing even a relatively low alcohol overconsumption as a major risk factor for developing DD. Furthermore, several previous studies have proposed manual work as a risk factor for the development of DD8, possibly through repeated microtrauma to the hand30. We found, however, no such associations in our study, neither among men or women, possibly due to the low number of farmers in the study population.
BMI and apolipoproteins
The epidemiological literature on circulating lipids, apolipoproteins and risk of DD is scarce, and the most cited papers date back to the 1980’s and 1990’s14,15. In recent years, however, an inverse association between a high BMI and the risk of DD have been reported in several studies11,12,31, indicating a possible protective factor linked to the fat tissue. The putative biological mechanisms behind this associations is not known but lower serum testosterone among obese individuals has been proposed as one hormonal factor of importance, possibly decreasing the risk for DD31. In our study, we found a similar pattern of associations; men with incident DD during follow-up had a lower mean BMI at baseline compared to men without DD. Additionally, obese men had lower risk of DD compared to men with normal weight in the adjusted regression model, although the same results could not be convincingly shown among women.
However, we did find a strong association among both men and women between apolipoprotein levels and incident DD. Participants with a high ApoB/ApoA1 ratio had a lower risk of DD even when adjusting for age, DM, alcohol consumption, and BMI. Traditionally, the ApoB/ApoA1 ratio has been used as a predictor of cardiovascular disease32,33 and analysis of ApoB is still recommended as a complement or alternative to LDL-C in risk assessment of cardiovascular disease34. Our study is to the best of our knowledge the first to analyze apolipoprotein levels in relation to DD, why further studies are warranted, firstly to confirm these results, and secondly to better understand the biochemical background to the reported associations. Interestingly, recent genetic studies have proposed a negative genetic correlation between high BMI and DD13, supporting the previous results associating lower BMI with DD11,12. Furthermore, in studies on over 30,000 Danish twin pairs, the hereditability of DD was approximately 80%, whereas environmental risk factors, e.g. smoking or alcohol consumption, only contributes to 20% of the increased risk9. A recent Swiss study found that family history of DD was a strong risk factor for incident DD, emphasising the importance of genetic susceptibility for the development of the disease35. This could indicate that the associations found between apolipoproteins, low BMI and DD are due to genetic correlation rather than fat tissue being protective against DD. Since no genetic information was available in this study, we cannot draw any conclusions regarding such associations from our results, but it is an obvious target for future studies. Another future research target would be to examine palmar fascia biopsies from overweight and obese patients with and without DD, aiming to better understand the interplay between BMI, fat tissue, and DD risk.
To summarize, there might exist different protective and predisposing factors for the development of DD. Genetic predisposition, hormonal factors related to sex or high BMI, alterations in the palmar fascia due to DM and hyperglycemia, and finally, environmental factors such as alcohol consumption all interact in the complex pathogenesis behind DD (Supplementary Fig. S1).
Strengths and limitations
One of the limitations of this study is the lack of standardized diagnostic criteria for DD during follow-up. The diagnoses were retrieved using ICD-codes and thus, physicians might have applied different criteria for diagnosis. Since we only used diagnoses from a specialized care setting, however, most diagnoses were established by trained specialists in hand or orthopedic surgery, strengthening case validity. Some participants might have been diagnosed with DD in primary care without specialist referral, which might have lowered our incidence rates to some extent. Indeed, data on incidence rates in our study are slightly lower than in a previous study from southern Sweden including data from primary care4, indicating that not all patients in Sweden with DD are referred to specialized care. Furthermore, since DD is a benign disease, some participants with moderate symptoms might not have sought healthcare at all despite having the disease and were thus not included in our registers. Taken together, our study design allowed us to analyze a clinically relevant diagnosis of DD, established in the specialized care setting, why results should be interpreted with this in mind. Another strength of this longitudinal study design is the lack of recall bias among participants, something that may otherwise be problematic in case–control studies.
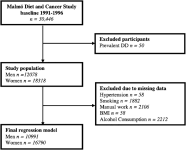
Furthermore, a major strength of this study is the large population size, over 30,000 middle-aged individuals followed over 20 years making this the largest cohort study to date analyzing risk factors for DD. Moreover, the collection of baseline data was of high quality, with each participant being examined individually by a trained nurse. The data regarding prevalent DM are also of high quality, using several local and national registers for diagnosis acquirement. Unfortunately, we were not able to reliably stratify for type 1 and type 2 DM, making separate analyses for different types of DM a target for future research. Levels of glycemic control (HbA1c) in relation to DD risk would also be an interesting topic for research. Finally, a participant’s baseline characteristics, such as BMI and alcohol consumption, were only measured once. Undoubtably, these variables often change over a person’s lifetime, and this is a limitation that should be kept in mind when interpreting our results.
Even so, despite the high quality of baseline data and our adjustments for known confounders in the regression models, there is always a possibility that additional confounders might have influenced our results. With all this in mind, our conclusions are in line with several previous studies indicating both DM and excessive alcohol consumption as risk factors for the development of DD, thus making it unlikely that residual confounding would be sufficient to alter our main results significantly, but caution should always be taken when interpreting data from observational studies.



